Intervertebral Disc
Disease in Dogs
Back to Fact Sheets
Intervertebral disc (IVD) disease in dogs is a common disorder of the spine.
Download PDF
Intervertebral disc (IVD) disease in dogs is a common disorder of the spine which could manifest with
- Pain;
- gait abnormalities such as ataxia (lack of coordination), paresis (reduced limb/limbs movement) or paralysis (absent limb/limbs movement);
- loss of sensation/feeling in the paralysed limbs (in the most affected cases).
IVD disease can affect the neck, thoracic and lumbar region and the junction between spinal regions (thoracolumbar and lumbo-sacral).
It occurs most frequently in chondrodystrophic breeds such as the Dachshund, Bull dogs, Pugs, Cocker Spaniel, Shih Tzu, Basset Hound and others. IVD disease can also occur in other non-chondrodystrophic breeds such as the German Shepherd, Labrador Retriever and many others.
The IVD is located between each vertebral body. The normal IVD consists of
- a hard, fibrous outside ring (the annulus fibrosus) containing
- a soft gel-like centre (the nucleus pulposus).
The function of the IVD is to connect the vertebral bodies and to act as a shock-absorber during every movement. Degeneration of the IVD occurs when the nucleus pulposus becomes dehydrated making the IVD unable to act as a good shock-absorber. In the chondrodystrophic dog, degeneration of the IVD begins between 2 and 10 years of age. 75% to 100% of all IVDs have undergone degeneration in the chondrodystrophic dog by 1 year of age. A different type of IVD degeneration occurs in non-chondrodystrophic dogs; this is a progressive slow aging process most evident between 8 and 10 years of age, due to abnormal hypertrophy of the annulus fibrosus.
IVD disease causes clinical signs when extrusion of the disc (the degenerated nucleus pulposus pushes its way into the spinal canal through the annulus fibrosus tear) or its protrusion (hypertrophy of the annulus fibrosus) compresses the overlying neural structures (spinal cord and/or spinal nerves) (Fig.1 and 2). Sometimes, especially during exercise, a normal nucleus pulposus can explode into the spinal canal hitting the spinal cord with a significant force causing bruising of the overlying spinal cord segments (Acute Nucleus Pulposus Extrusion) (Fig.3).
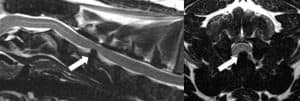
Fig.1: Midline sagittal T2W MR image of the cervical spine (left) and transverse T2W MR image at the level of the C4-C5 IVD (right) of a 3yr MN French Bulldog presented for ambulatory tetraparesis and severe neck pain showing a C4-C5 IVD extrusion severely compressing the spinal cord (arrows). All intervertebral disc are degenerated (dark on MRI).

Fig.2: Midline sagittal T2W MR image of the thoraco-lumbar spine (left) and transverse T2W MR image at the level of the T12-T13 IVD (right) of a 10y MN Staffordshire Bull Terrier presented for assessment of a long history of progressive paraparesis and pelvic limb ataxia showing a T12-T13 IVD protrusion compressing the spinal cord (arrows).
Clinical signs
Clinical signs are dependent on the location of the lesion affecting the spinal cord. Dogs might display anorexia, abnormal spinal kyphosis, a tense abdomen or yelping when moving or when they are picked up. Other signs include shivering or trembling, reluctance to move and scuffing/dragging/spontaneous knuckling of the paws. In the more extreme cases, the dog will completely lose the ability to move the limbs. Dogs with IVD disease in the cervical region frequently hold the head down when walking, have muscle spasms in the neck and will cry in pain when the cervical spine is moved.
Diagnosis
As for many diseases, an early diagnosis can significantly improve the chances of recovery.
The diagnosis of IVD disease is made using combination of
- physical and neurologic examinations;
- advanced imaging of the spine such as CT or, more reliably, MRI of the spine. In some instances, a myelogram/CT myelogram could be performed by injecting a contrast medium around the spinal cord and then making additional radiographs to demonstrate the location of the IVD disease.
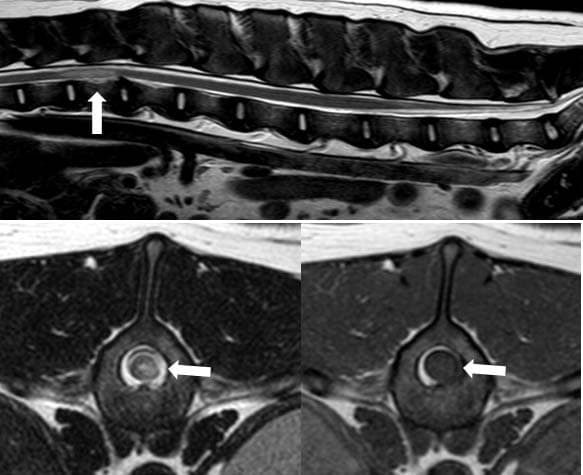
Fig.3: Midline sagittal T2W MR image of the thoraco-lumbar and lumbar spine (top), transverse T2W MR image (bottom left) and transverse T1W MR image (bottom right) at the level of the T13 vertebral body of a 7y ME Labrador presented for a peracute onset of left pelvic limb monoplegia and right pelvic limb monoparesis occurred whilst chasing a ball. (arrows). Note the increased T2W intramedullary signal intensity (arrow on top image and on bottom left image) lateralised to the left compatible with spinal cord contusion. Non compressive extruded IVD material is noticed surrounding the spinal cord on the left side (arrow on bottom left and bottom right images).
Treatment & Aftercare
The most appropriate treatment can be recommended after achieving an accurate diagnosis of IVD disease. Medical management, surgical management and their combination seek to alleviate the pain and any other neurologic deficits associated with IVD disease. Many paralysed patients, even if they have lost nociception in the limbs, can often be helped. However, when a condition termed myelomalacia (spontaneous haemorrhagic cellular death in the spinal cord) develops, the prognosis becomes hopeless.
Medical treatment is indicated for
- patients only manifesting pain or mild loss of limb function;
- if investigations/ additional treatment is not affordable;
- in patients with a high anaesthetic risk;
- when diagnostic tests do not show spinal cord compression.
Medical treatment includes
- very strict confinement in a confined area (ideally a transportation crate) with plenty of soft, absorbent padding. Regular toilet breaks for a very short period are generally allowed;
- Pain relief administration (such as a NSAID—non–steroidal anti–inflammatory drug and/or gabapentin); muscle relaxant might also be administered in specific cases.
- Acupuncture may also provide pain relief for some patients;
- If a patient is not able to voluntarily urinate, manual bladder expression should be performed every 6 hours.
Surgical treatment is indicated anytime the spinal cord is compressed by extruded/protruded IVD, when the patient is showing severe pain and when a patient has relapsed clinical signs despite appropriate medical management. Surgical treatment consists of the removal of the extruded/protruded IVD material compressing the spinal cord. It can be highly successful in the hands of a trained veterinary neurosurgeon and its advantage over medical treatment is the complete removal of the extruded/protruded IVD and the rapidity of recovery. The average post-surgical hospitalisation ranges between 2 days and about one week. After surgery, or after recovery following medical treatment, physiotherapy might be advised. This can range from simple exercises performed at home by the owner to a program that includes specialist physiotherapy and hydrotherapy needing specialist facilities.
Prognosis
IVD disease is not a fatal condition, except in those patients who develop myelomalacia. Earlier treatment generally results in a better outcome. Dogs with minimal to no neurologic deficits and well controlled pain usually have a fair to good prognosis for recovery with medical treatment. About a third of the patients treated medically might relapse, needing further advanced diagnostic imaging and, eventually, surgical management. Dogs with more severe signs, with a severely compressed spinal cord with nociception in the affected limbs have a good to excellent prognosis for recovery after a successful surgery.
For dogs with more severe signs, with a severely compressed spinal cord and without nociception, the prognosis for recovery of neurologic function begins to significantly decrease and surgery should be performed on these patients as soon as possible to maximise the chances of recovery. For these patients, recovery can occur even up to two months after the onset of clinical signs. Some dogs that do not recover sensation or other neurologic functions can be maintained with an acceptable quality of life using carts and having the owners assist them with bladder expression.


