Meningo-encephalomyelitis of
Unknown Origin (MUO)
Back to Fact Sheets
MUO is thought to be an immune-mediated condition. For reasons that are currently unknown, the immune cells target the body’s own cells.
Download PDF
What is MUO?
- Meningitis means inflammation of the meninges (the thin layers of tissue surrounding the brain and spinal cord).
- Encephalitis means inflammation of the brain.
- Myelitis means inflammation of the spinal cord.
- The exact terminology used depends on what structures are affected in a particular case. For example, meningomyelitis would mean that the meninges and spinal cord are inflamed.
- In animals affected by MUO, inflammatory cells that are normally involved in immune responses, such as fighting off infection, move from the bloodstream into the central nervous system. This causes inflammation in the brain, spinal cord, or meninges.
- MUO is thought to be an immune-mediated condition. For reasons that are currently unknown, the immune cells target the body’s own cells.
- Despite extensive research, no underlying reason has been identified that can explain why particular animals are affected by MUO. Some breeds appear to be more commonly affected than others, suggesting at least a component of genetic susceptibility, but at present the underlying cause is not understood.
- Further categorisation of MUO can be achieved if a piece of diseased tissue is analysed at the laboratory. Depending on the type and exact location of the inflammatory cells, the disease process might be classified as granulomatous meningoencephalomyelitis, necrotising encephalitis or leukoencephalitis. It is uncommon for a sample to be taken from the brain or spinal cord of a live animal so these very specific terms are not frequently applied to our patients.
- Instead, the broad term MUO is generally used to refer to all the subtypes of the condition.
What clinical signs (symptoms) occur in cases of MUO?
- The clinical signs in cases of MUO are very varied. The type and severity of abnormalities depend on the location and degree of the inflammation. Dogs with inflammatory lesions in the brain, for example, may present with seizures and behaviour change, whereas those with lesions confined to the spinal cord may show abnormalities in their walking. It is not uncommon for lesions to be spread throughout the central nervous system, causing a range of abnormalities. The clinical signs also vary greatly in their severity. Some dogs may show subtle signs such as vague discomfort, whereas others can have dramatic abnormalities such as very abnormal mental status or inability to walk.
How is MUO diagnosed?
- The age and breed of the affected dog may give a clue- MUO most commonly affects young to middle aged smaller breeds of dog. Females are more commonly affected; it is not known why this is the case. However, any age, breed and sex of dog can be affected. MUO is very rare in cats.
- The history is typically of progressive, sometimes waxing and waning neurological abnormalities. The signs are usually seen to develop gradually over a few days. In rare cases the clinical signs occur very suddenly.
- A general and neurological examination will be performed to determine that the problem is of neurological origin and which parts of the nervous system are likely to be affected.
- Blood tests will often be performed to give an overview of the patient’s general health, to look for any signs of disease elsewhere in the body and to ensure that procedures such as general anaesthesia and administration of medications are safe.
- The brain and/or spinal cord are likely to be imaged using MRI. While there are not imaging features that are absolutely definitive for diagnosing MUO, particular characteristics of the MR images add to the overall evidence that a particular patient is affected.
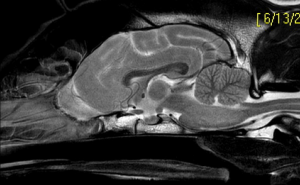
Sagittal T2 image of the brain of a dog with Granulomatous meningo-encephalitis showing a lesion in the brainstem
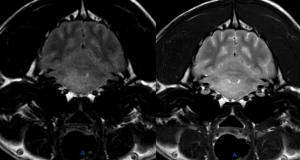
Transverse FLAIR and T2 image of the brain of a dog with Granulomatous meningo-encephalitis showing the same lesion in the brainstem
- A cerebrospinal fluid (CSF, the fluid that bathes the brain and the spinal cord) sample will sometimes be obtained. The CSF of dogs with MUO will often contain an increased number of inflammatory cells, as well as increased protein. The analysis also helps to rule out other diseases, such as some tumours, that can look similar to MUO on the MRI. The CSF is also checked for any sign of infection. The decision whether to sample CSF will always be made after the MRI as in some cases the MRI will show us that it is not safe to obtain a CSF sample.
- Both MRI and CSF sampling require general anaesthesia.
- The patient will usually be tested for some infectious diseases (either by a blood test or using the CSF) that can cause central nervous system problems.
- If a patient’s history, clinical signs, bloodwork, MRI and CSF are compatible with MUO, and infectious disease is ruled out, a presumptive diagnosis of MUO is made. The term ‘presumptive’ is used simply because a definitive diagnosis made by analysing a sample of diseased brain or spinal cord in the laboratory is not usually possible in the live animal.
What treatment is required?
- As the disease is thought to be immune-mediated, treatment is focussed on suppressing the immune system.
- This can be done using a variety of medications.
- Corticosteroids (also termed steroids) are used in almost all cases of MUO. These are a different type of steroids to anabolic steroids that bodybuilders use. Corticosteroids are used as anti-inflammatories at lower doses and immunosuppressives at the higher doses used for MUO. They are effective, fast-acting and inexpensive. They are usually given as an injectable form initially, then as an oral form (usually prednisolone) at home. Common side-effects of corticosteroids include drinking and urinating more and feeling hungrier than usual. Your pet will almost certainly show these effects at the doses required for MUO treatment. Dogs receiving corticosteroids do not require more calories; they should be fed their usual diet even if they seem hungry. Vomiting and diarrhoea can be seen. Giving the medications with food, rather than on an empty stomach, may reduce the chances of gastrointestinal upset. Please contact us in the event of problematic vomiting or diarrhoea. Long-term corticosteroid administration can result in a thin and dry coat, a pot belly and increased susceptibility to infections. Female dogs may have irregular oestrus cycles.
- There is good evidence that using a second immunosuppressive drug, alongside prednisolone, improves outcome in MUO cases. Drugs that may be used include cytarabine, cyclosporine and procarbazine. Each of these drugs has particular advantages and disadvantages, associated costs and possible side-effects (which are not very common or severe). Some are given at home, orally, whereas others (for example cytarabine) are given by injection. The neurologist treating your pet will discuss these medications with you and be able to make a recommendation on a case-by-case basis.
- Medications will be required long-term. The dosages are gradually reduced over time with the aim to keep the disease in remission but minimise adverse effects from the drugs. This is typically a very slow process over many months. Most dogs remain on medications for the rest of their lives, though these can often be reduced to very low doses.
- It is very important that medications are not modified in any way without speaking to a veterinary neurologist first.
What is the prognosis?
- MUO is a serious disease and sadly has been reported to be fatal in up to a third of cases.
- Even with gold-standard treatment, some animals do not recover.
- The prognosis is considered guarded in the first three months or so of treatment, but dogs that show a good response to treatment during this time frame often go into prolonged remission and can enjoy an excellent quality of life.
- Some dogs, especially those that have been very severely affected, may have permanent neurological deficits.
- Relapse of the disease can occur. If you suspect recurrence of the clinical signs please contact us without delay.
- Discontinuation of immunosuppressive treatment should only ever be considered if MRI and CSF sampling have been repeated and found to be normal.
- Vaccination may trigger relapse of MUO. This is because vaccinations work by stimulating the immune system, which in MUO patients may respond abnormally or excessively. It is recommended that MUO patients do not receive annual booster vaccinations. Under these circumstances it is safest to ensure that your dog only mixes with other dogs you know to be fully vaccinated. Swimming in rivers, streams and ponds should not be permitted as these can be a potential source of infectious disease.
- Flea and worming treatments can be given as normal.


