Radiotherapy for
Apocrine Gland Anal Sac Adenocarcinoma (ASAGA)
Back to Fact Sheets
What is ASAGA and when do you advise radiotherapy?
Download PDF
What is ASAGA and when do you advise radiotherapy?
ASAGA is a tumour which arises from the glands that line the anal sacs. The anal sacs are two small sacs that sit at approximately 4 o’clock and 8 o’clock in position around and just inside the anus. They produce some fluid and commonly get blocked in some pets, causing dogs to classically scoot their bum along the ground. ASAGA develops from these glands and so dogs typically develop a firm lump at around the 4 o’clock or 8 o’clock position. In most cases, this is on one side only (unilateral), but can be bilateral (both anal sacs affected – either at the same time or affected separately).
Some patients with ASAGA have a tumour that is confined to the anal sac(s). These tumours do have a high risk of spreading (metastasising) to nearby lymph nodes in the pelvis/belly. This can either be present at the time of diagnosis, or it can develop later on after initial diagnosis; sometimes even years later.

The tumour is split into stages depending on the tumour site and extent of spread:
- Stage 1: anal sac tumour <2.5cm and no spread detected on scans
- Stage 2: anal sac tumour >2.5cm and no spread detected on scans
- Stage 3a: anal sac tumour of any size and spread to lymph nodes which are <4.5cm
- Stage 3b: anal sac tumour of any size and spread to lymph nodes which are >4.5cm
- Stage 4: anal sac tumour of any size and spread to distant sites

Stage 1 and 2 tumours are predominantly treated with surgery. If possible, it is reasonable to treat these patients with surgery alone (to remove the anal sac tumour itself) followed by “active monitoring” to check for any local recurrence of the tumour (recurrence around the bum, at the surgical site) or spread to internal lymph nodes (as detailed earlier). This can be done with a combination of regular physical/rectal examination, ultrasound or CT scans. Further treatment can be performed in the cases where the tumour progresses.
In cases where the surgery was particularly difficult and/or the tumour was very large, or not completely removed, further treatment such as radiotherapy may be recommended to try and reduce this risk by eradicating the residual tumour cells. If this is performed, it is normal for us to “preventatively” treat the nearby lymph nodes also, because this is such a common site of later spread.
The outcome for dogs with stage 1-2 tumours can be 2-3 years or longer, on average. Of course, some pets don’t do as well as their tumour progresses unusually quickly – but this is rare.
ASAGA can progress years after initial successful treatment, so long-term monitoring with regular rectal examinations and imaging studies (e.g. ultrasound and x-ray/CT) is strongly recommended.
Because there is at least a moderate risk of this tumour recurring at the primary site near the anus and in the nearby lymph nodes, we will offer radiotherapy to the primary site and lymph nodes after surgery, for owners that wish to pursue a more intensive and “proactive” treatment path. At least in theory, early treatment of cancer can be more successful and may be more likely to be curative.
The options of “active monitoring” after surgery versus “up front” radiotherapy (RT) will have been discussed by your oncologist at the time of consultation.
Stage 3a/3b tumours can also be treated surgically (surgery to remove the primary tumour around the bum and also surgery to remove the cancerous lymph nodes via a midline incision in the belly). However, surgery is not always possible as these tumours are usually large and sometimes the lymph nodes are stuck to important blood vessels internally or other structures that can make surgery tricky, risky or impossible.
In cases where surgery alone is performed, the outcome is not as promising; with the tumour tending to recur after around 4-6 months and “average” survival times being around 11 months. Therefore, these are cases where we strongly advise RT after surgery, rather than “active monitoring” with the expectation that this will prevent or at least delay the tumour from recurring in other lymph nodes nearby.
It is also reasonable to use RT as the primary/sole treatment for stage 3 (a or b) ASAGA, as the outcomes with RT alone reported so far are very good. In one study, the majority of dogs with stage 3 tumours that had RT lived for > 1 year (and overall, on average, >2 years). We see many stage 3 patients that live for 1-2 years+ with RT alone.
In theory, removing as much disease as possible surgically (i.e. in stage 3 patients removing the primary tumour and also the lymph nodes) is beneficial as the RT has “less work to do” and may therefore work better and be more likely to eradicate as possible. However, we can’t say for sure how much benefit surgery has compared with RT alone, and surgery is an invasive procedure. Therefore, this is something that will have been discussed during your consultation. How much surgery is recommended by your oncologist may depend on factors such as your desire to treat aggressively, the size or number of the tumour(s), scan results, any symptoms associated with the tumour and the presence of high calcium levels.
Stage 4 tumours tend to be treated with palliative intent, as they have already spread to distant sites such as the liver or lungs or multiple places. These tumours tend to be treated with chemotherapy alone, such as the newer drug toceranib phosphate (Palladia). This can shrink tumours in around 20% of cases and in many more patients stabilise the tumour and delay its progression. There are some side effects, but these can usually be well managed with appropriate monitoring and tailoring of the dose to the individual pet. ASAGA tends to progress slowly in most patients, so particularly if there are only a couple of metastases (e.g. one or two small lung nodules), RT may still form part of the treatment; particularly if a pet is suffering from symptoms relating to the primary tumour or lymph nodes (e.g. constipation). In those types of cases, RT is usually less intensive, to avoid frequent visits and more intense side effects in pets with a poorer long-term outcome.
Because ASAGA can progress quite slowly, if tumours only progress in one or two places (e.g. a lung nodule or a liver nodule) and the patient is still medically fit and well, we may even be able to “spot treat” these lesions with a highly focussed type of radiation (stereotactic radiation; SRT). There is some evidence in humans that slowly spreading tumours can be managed well this way.
With treatments such as palliative-intent radiotherapy to manage the primary tumour/lymph nodes (if needed) and drugs like Palladia, some dogs with stage 4 ASAGA can live for many months and in some cases a year or more.
High calcium levels and ASAGA
Some ASAGA tumours produce a hormone called PTHrp that tricks the body into increasing calcium levels to above-normal limits (hypercalcaemia). This can cause increased thirst and urination, but sometimes no major signs are noticed. Sometimes dogs just seem “under the weather” when their calcium is high. Hypercalcaemia is best resolved with treatment of the underlying tumour and most rapidly resolved with surgery. If surgery is not an option, radiotherapy can help reduce calcium levels but as RT works slowly, medical treatment may be needed in the meantime. As palliative treatment, medications can help with calcium levels. This must be managed, as chronically high calcium can affect the kidneys.
Radiotherapy for ASAGA
Radiotherapy is becoming increasingly available and is much more targeted than it was previously, meaning safer and more effective treatments with significantly fewer short and long-term side effects. Recent studies suggest that when radiotherapy is used, the outcome can be very good and better compared to surgery alone (particularly for high-stage tumours), chemotherapy or no treatment.
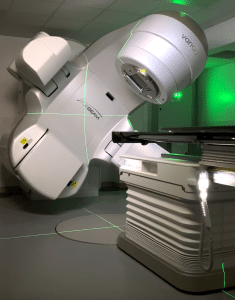
Radiation therapy (also called radiotherapy; RT) involves treatment with high-energy X-rays, the aim being to kill the tumour. We use a machine called a linear accelerator. Patients lie on the treatment couch and the machine delivers a focussed beam of X-rays from multiple angles 360° around the patient.
Radiation for ASAGA can be performed with definitive intent (meaning we are trying to give the biggest dose possible to try and get the best outcome) or with palliative intent (lower dose/less frequent radiation treatments to try and improve symptoms whilst avoiding side effects, but without the expectation of long survivals).
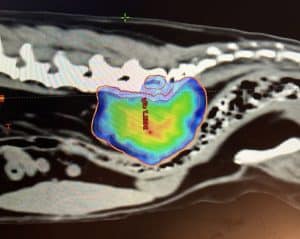
Each radiation treatment is performed under a short, light general anaesthetic. Prior to the start of treatment, a planning CT scan will be needed to help us prepare a bespoke plan for your pet. This helps us to maximise the radiation dose to the tumour whilst sparing the nearby tissues. This will be required even if your pet has had a recent CT scan, as we need patients to be in a very particular and fixed position so that the treatment can be carried out with pinpoint accuracy.
Unfortunately, even with radiotherapy, we usually cannot cure your pet’s tumour. However, radiotherapy can be a very satisfactory treatment for improving quality of life, reducing the risk of side effects and controlling the tumour. RT is well tolerated by most patients; particularly with newer technologies to help avoid side effects and in many cases make treatment courses much shorter.
Does ASAGA spread to other places in the body?
ASAGA can spread (metastasise) to other sites in the body (such as lymph nodes nearby, lungs, and liver). In particular, the first site of tumour spread is almost always the sublumbar lymph nodes, just inside the belly. Before deciding on the best course of treatment, we need to know the tumour stage. We typically recommend at least a chest (thorax) CT at the time of your pet’s abdominal/pelvis planning CT scan (performed to plan RT). Luckily, extensive tumour spread at the time of initial diagnosis is not common. Specific additional tests may be recommended based on your pet’s individual case.
Will my pet’s tumour-related symptoms improve after RT?
ASAGA is sensitive to radiotherapy, though the response can be different for each patient.
The full effect of the treatment may be slow and can take weeks or even months for the tumour to slowly shrink to the smallest size. Some tumour types shrink more slowly and shrink less. In some patients, we might only be able to stop it from growing further. In these patients, the benefit may not be as obvious as there will be less improvement in symptoms.
The hope is that as most tumours at least stop growing, any symptoms will not get any worse (whilst the tumour is under control). Many tumours do shrink with RT, so we hope that the risk of any symptoms relating to the tumour will improve. Overall, we would expect at least two-thirds of patients to get a big improvement in their symptoms if they have any.
Radiotherapy Protocols
There are several different types of radiotherapy protocols that we generally offer for dogs with ASAGA:
- Fractionated Radiation Therapy (FRT; this is the most conventional type of radiotherapy).The total radiation dose is split into multiple small treatments (called fractions) to ensure the radiation is not too damaging to any normal tissues around the tumour in the long term (mainly the bladder and intestine). This treatment usually consists of 16-20 fractions, each given once a day (not weekends), over 3-4 weeks. If needed, we can use intensity-modulated radiation therapy (IMRT) – a type of RT delivery which means we can significantly avoid radiation dose to the normal structures around the tumour. This means the degree and severity of acute side effects are reduced from what we used to see historically (see below). Because the treatment is delivered in multiple smaller doses, the risk of late effects (see later), particularly to the colon/rectum, is lower. The goal of these types of protocol are to try and achieve the best and longest tumour control possible (i.e. “definitive-intent” therapy).
- Stereotactic Radiation Therapy (SRT). This is a newer type of radiotherapy technique which has come about due to significant technical developments in radiotherapy over the last few years. SRT usually consists of 3-5 treatments delivered once daily over 3-5 consecutive days (Monday to Friday; there are no treatments at weekends). For some tumours, this protocol may be spaced out over a slightly longer time period (e.g. every other day over 2 weeks). It is a highly focused technique with the goal of treating the tumour but as little surrounding normal tissue as possible. The risk of significant acute side effects (see below) associated with this protocol is low. The risk of late side effects is at least the same as with fractionated radiation, if not potentially higher due to the high radiation dose given with each treatment. Therefore, this technique may not be possible for all tumours – particularly those that are very large, are not well-defined, have lots of surrounding inflammation or lie against a large volume of intestine.
Stereotactic radiation is uncommonly used for ASAGA because the outcomes are very good with conventional FRT, but also because of the area treated. Given the lymph nodes in the belly are the most common sites for tumour relapse, we treat a very wide/broad area where the lymph nodes sit, in a large strip under the spine heading from the pelvis towards the kidneys. This is not possible to treat with SRT.
SRT can be used where there is a well-defined disease which can be targeted, such as a large primary tumour and/or some large lymph nodes, but with the knowledge that we are not treating a lot of “at-risk” tissue in other areas.
- Palliative radiation therapy – this is where we give a low/modest dose of radiation to try and provide an improvement in symptoms but with relatively short protocols and with little short-term (acute) toxicity. The goal/expectation is not long-term survival but to try and make pets more comfortable for the time they have left. Most protocols are once per day for 5-10 consecutive days, or once per week for 4-6 weeks. Sometimes the choice is based on tumour size/location/type and sometimes is based on owner preference.
- Individual protocols: may be recommended in certain situations, for example, due to a patient’s concurrent medical conditions, owner logistics or pet temperament.
Potential side effects related to radiotherapy:
Acute side effects (predictable and temporary)
- Hair loss (alopecia) in the treated site: around the anus/tail base
- Sore skin (radiation dermatitis): Most severe with FRT – tends to occur towards the end of treatment, get worse for a week or so then heal over 2-3 weeks. Can be pretty raw and moist, becoming oozy and then crusting over before healing
- Colitis/proctitis and diarrhoea (inflammation of the colon/rectum):will occur to some degree in most pets receiving FRT. Symptoms may include straining to pass a stool, some fresh blood in the stool, mucus in the stool or scooting the bum along the ground. This can be quite sore but is temporary and manageable. Given the location, this is very common with SRT too – but mostly low-grade toxicity
- Death: This is exceptionally rare, but pets can suddenly deteriorate during treatment; e.g. due to anaesthesia complications (e.g. aspiration pneumonia) or other medical conditions
Delayed complications – these are uncommon and typically arise from 3 months after a course of radiation is completed (usually after 6 months or sometimes years after treatment completion). Serious complications such as strictures are rare with FRT (risk ~2-4%)
- Leukotrichia or melanotrichia: white or black hair regrowth/altered skin pigmentation in the radiotherapy treatment site is normal. Hair loss in the treated site around the bum/tail base
- Stricture (colon/rectum): narrowing of the colon/rectum which may cause difficulty passing a stool/straining. May need dilating and anti-inflammatory medication or other therapy – this is uncommon with FRT but is potentially more of a risk with SRT
- Chronic colitis (colon inflammation) which could cause straining to pass stool
- Radiation-induced tumours: an exceedingly rare complication (typically seen years after initial treatment) and is usually the development of a tumour arising within the treated site
The goal of radiotherapy is to reduce the risk of serious late side effects as much as possible – we aim for <5% overall however in certain individuals the risk may be higher (this will be discussed by your oncologist). The risk may be higher or not fully known, particularly in cases where a relatively novel technique is being used or where SRT is being utilised.
Chemotherapy:
Traditional chemotherapy is not very effective for ASAGA, though it has been used for a long time either as a palliative treatment or after surgery to try and prevent tumour spread. To date, there are no studies proving any real benefit to the administration of chemotherapy to ASAGA patients as part of first-line treatment. It can, however, show some usefulness as palliative treatment for patients with advanced disease or where other treatments have been used and failed.
Toceranib phosphate (PalladiaÔ) has shown some usefulness in ASAGA patients and tends to be used where radiotherapy has been declined or was inappropriate/ineffective. We may also recommend alongside palliative-intent RT.
Palliative Care:
Should you not wish to proceed with any anti-cancer treatment, palliative care should be considered. Palliative care is where we treat the symptoms associated with the tumour without giving any direct anti-cancer treatment. We often recommend anti-inflammatories (NSAIDs) and/or painkillers, but the exact treatment will depend on the symptoms that your dog has.
What about cats?:
There is much less information about ASAGA in cats as it is rare. However, the general principles are similar and so the recommended treatment plan is likely to be similar.