Radiotherapy for
Bladder/Urogenital Tumours
Back to Fact Sheets
The most common type of tumour we treat is transitional cell carcinoma (TCC)
Download PDF
What type of urogenital tumours do you treat? Is surgery useful?
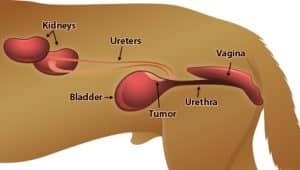
The most common type of tumour we treat is transitional cell carcinoma (TCC) of the urinary bladder, urethra (the tube that takes urine from the bladder to the outside) and prostate. It can affect one or all of these regions.
Symptoms may include blood in the urine, straining to pass urine, urinary accidents or urinating much more frequently. Particularly with prostate tumours, straining to pass stools can also occur.
TCC of the bladder is the most common. TCC mostly affects the trigone region of the bladder. The trigone is the neck of the bladder, where urine enters the bladder from the kidneys (via two tubes called the ureters) and urine exits the bladder into the urethra. There are also lots of important blood vessels and nerves in this region. For that reason, surgery is rarely performed as it is risky, carries a high degree of significant complications and has a high rate of permanent incontinence. For similar reasons, when the prostate is affected, removal of the prostate is rarely recommended. These tumours are also pretty diffuse – it is often difficult to appreciate where they start/stop (even on ultrasound or CT scans) which is another reason surgery is often not considered.
Surgery can be a very good option for tumours at the “apex” of the bladder (away from the trigone) and outcomes can be very good, particularly when post-op anti-inflammatories (NSAIDs) are given. In such cases, we may even just monitor with serial ultrasound scans rather the provide further local treatment (e.g. radiotherapy) and just consider more treatment when the tumour recurs. Even in cases where surgery is performed, recurrence after a few months is common as these tumours often diffusely affect the bladder/urinary tract beyond what can be detected surgically or on imaging studies.
However, most dogs with TCC present with tumours that are not amenable to surgery and so treatments such as radiotherapy and chemotherapy are considered good options for these patients.
Radiotherapy for urogenital tumours: is it the only option?
As described above, surgery can be used for a small number of cases, but for most pets with TCC this is not a good option.
Radiotherapy is becoming increasingly available and is much more targeted than it was previously, meaning safer and more effective treatments with significantly fewer side effects. Recent studies suggest that when radiotherapy is used, the outcome can be very good and better compared to chemotherapy alone or no treatment.
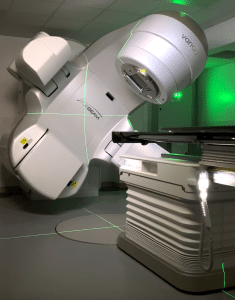
Radiation therapy (also called radiotherapy; RT) involves treatment with high-energy X-rays, the aim being to kill the tumour. We use a machine called a linear accelerator. Patients lie on the treatment couch and the machine delivers a focussed beam of X-rays from multiple angles 360° around the patient.
Radiation for TCC can be performed with definitive intent (meaning we are trying to give the biggest dose possible to try and get the best outcome) or with palliative intent (lower dose/less frequent radiation treatments to try and improve symptoms but without the expectation of long survivals).
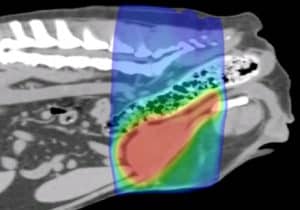
Each radiation treatment is performed under a short, light general anaesthetic. Before the start of treatment, a planning CT scan will be needed to help us prepare a bespoke plan for your pet. This helps us to maximise the radiation dose to the tumour whilst sparing the nearby tissues. This will be required even if your pet has had a recent CT scan, as we need patients to be in a very particular and fixed position so that the treatment can be carried out with pinpoint accuracy.
Unfortunately, even with radiotherapy, we usually cannot cure your pet’s tumour. However, radiotherapy can be a very satisfactory treatment for improving quality of life, reducing the risk of side effects and controlling the tumour. RT is well tolerated by most patients; particularly with newer technologies to help avoid side effects and in many cases make treatment courses much shorter.
In bladder tumours, changes in the volume of urine within the bladder can also cause an issue, as the size of the bladder needs to be as close as possible to the size at the time of the planning CT scan. We perform a mini CT scan prior to treatment to check the size of the bladder as part of patient positioning. Sometimes we have to place a urinary catheter to suck out some urine and sometimes we need to put some saline into the bladder to increase the bladder size or use intravenous fluids to help fill the bladder. We may do this every day or just on the same days. We try and treat patients at a similar time every day and after they’ve been to the toilet to urinate. Very rare risks of these procedures include introducing infection (though these patients are prone to urine infections anyway) or extremely rare rupture of the bladder/urinary tract from catheterising bladder already damaged by the tumour. The utmost care is taken to avoid these extremely rare complications. These issues of bladder “fullness” are less of an issue in patients receiving palliative RT as the lower doses given mean we don’t have to worry as much about this.
Non-steroidal anti-inflammatory drugs (NSAIDs) are important to use in pets with TCC as they can have direct anti-cancer action, as well as making pets feel better. By themselves, treatment is palliative.
Chemotherapy has been most widely used to treat dogs with TCC (alongside NSAIDs) to try and get a better outcome than with NSAIDs alone.
Radiotherapy is relatively new in terms of treating urogenital tumours in animals because of the rare and expensive equipment/expertise and specialised radiation equipment required. However, the more recent studies looking at RT (+/- chemotherapy and NSAIDs) have suggested the outcome for pets may be better than chemo/NSAIDs alone when RT is incorporated into the treatment plan.
Will any further tests be recommended prior to RT?
We may recommend an endoscopy (a small camera is placed inside the urinary tract to assess the extent of the tumour) so we can be sure we know where the tumour starts and stops. This will depend on the individual case.
Does TCC spread to other places in the body?
TCC often spreads (metastasis) to other sites in the body (such as lymph nodes nearby, lungs, and bone). We need to check that this has not occurred before we embark on a course of radiation for your pet. We typically recommend at least a chest (thorax) CT at the time of your pet’s abdominal/pelvis planning CT scan (performed to plan RT). Luckily, extensive tumour spread at the time of initial diagnosis is not common. Specific additional tests may be recommended based on your pet’s individual case.
Your pet may still be a candidate for RT if they have a tumour spread, but most likely the treatment course will be palliative.
Will my pet’s tumour-related symptoms improve after RT?
Bladder tumours are sensitive to radiotherapy, though the response can be different for each patient.
The full effect of the treatment may be slow and can take weeks or even months for the tumour to slowly shrink to the smallest size. Some tumour types shrink more slowly and shrink less. In some patients, we might only be able to stop it from growing further. In these patients, the benefit may not be as obvious as there will be less improvement in symptoms.
The hope is that as most tumours at least stop growing, any symptoms will not get any worse (whilst the tumour is under control). Many tumours do shrink with RT, so we hope that the risk of any symptoms relating to the tumour will improve. Overall, we would expect at least two-thirds of patients to get a big improvement in their symptoms.
Dogs commonly get urinary tract infections (UTIs) when they have TCC, due to their abnormal urinary tract. The symptoms of a UTI can be identical to tumour symptoms – so never just assume any worsening or recurrence of symptoms is tumour progression/relapse.
Radiotherapy Protocols
There are several different types of radiotherapy protocols that we generally offer for dogs with bladder tumours:
- Fractionated Radiation Therapy (FRT; this is the most conventional type of radiotherapy).The total radiation dose is split into multiple small treatments (called fractions) to ensure the radiation is not too damaging to any normal tissues around the tumour in the long term (mainly the bladder and intestine). This treatment usually consists of 16-20 fractions, each given once a day (not weekends), over 2-4 weeks. We almost always use intensity-modulated radiation therapy (IMRT) for bladder tumours: a type of RT delivery which means we can significantly avoid radiation dose to the normal structures around the tumour. This means the degree and severity of acute side effects are massively reduced from what we used to see historically (see below). Because the treatment is delivered in multiple smaller doses, the risk of late effects (see later), particularly to the bladder and colon/rectum, is lower. The goal of these types of protocols is to try and achieve the best and longest tumour control possible (what we call “definitive-intent” therapy)
- Stereotactic Radiation Therapy (SRT). This is a newer type of radiotherapy technique which has come about due to significant technical developments in radiotherapy over the last few years. SRT usually consists of 3-5 treatments delivered once daily over 3-5 consecutive days (Monday to Friday; there are no treatments at weekends). For urogenital tumours, this protocol may be spaced out over a slightly longer period (e.g. every other day over 2 weeks). It is a highly focused technique with the goal of treating the tumour but as little surrounding normal tissue as possible. The risk of acute side effects (see below) associated with this protocol is very low. The risk of late side effects are at least the same as with fractionated radiation, if not higher due to the high radiation dose given with each treatment. Therefore, this technique may not be possible for all tumours – particularly those that are very large, are not well-defined, have lots of surrounding inflammation or lie against a large volume of the intestine. Stereotactic radiation is uncommonly used for bladder tumours due to the potential risk of bladder/colon damage, damage to the ureters or urethra. Also many bladder tumours This is because of the high doses given per treatment and the intensity of the treatment. Also, the necessary precision of the treatment is difficult to ensure given the movement of the bladder and different shapes/sizes of the bladder every day. It MAY be possible to consider for rare well-defined tumours affecting a small region of the urinary tract, particularly if it appears to be in a less mobile site. It may be able to be considered as a 2nd option for patients deemed unfit to undergo a traditional longer course of RT.
- Palliative radiation therapy – this is where we give a low/modest dose of radiation to try and provide an improvement in symptoms but with relatively short protocols and with little short-term (acute) toxicity. The goal/expectation is not long-term survival but to try and make pets more comfortable for the time they have left. Most protocols are once per day for 5-10 consecutive days, or once per week for 4-6 weeks. Sometimes the choice is based on tumour size/location/type and sometimes is based on owner preference or logistics.
- Individual protocols: may be recommended in certain situations, for example, due to a patient’s concurrent medical conditions or temperament
Potential side effects related to radiotherapy:
Acute side effects (predictable and temporary)
- Hair loss (alopecia) in the treated site: very rare with bladder tumours and not expected – potentially more likely in tiny patients, particularly if they are a non-moulting breed. May occur over the belly wall, around the vagina or near the penis/groin
- Sore skin (radiation dermatitis): very rarely significant with bladder tumours – but around 25% will get some degree of dermatitis around the penis/vagina/groin or anus. Some dark skin pigmentation could appear in some dogs which may be long-term
- Colitis/proctitis and diarrhoea (inflammation of the colon/rectum):will occur to some degree in around 50% of pets – mostly low-grade. Symptoms may include straining to pass a stool, some fresh blood in the stool, mucus in the stool or scooting the bum along the ground
- Urinary side effects: some temporary worsening of urinary symptoms (straining, blood in the urine or passing blood clots) as the tumour starts to become inflamed and die off. It could also signal a UTI, which is common with or without treatment in dogs with TCC. Very rarely, this could result in urinary obstruction (inability to pass urine, which could be an emergency)
- Death: This is exceptionally rare, but pets can suddenly deteriorate during treatment; e.g. due to anaesthesia complications (e.g. aspiration pneumonia) or other medical conditions
In bladder tumour patients, these side effects are usually mild and rarely problematic these days. They are short-term, predictable and self-resolving.
Delayed complications – these are uncommon and typically arise from 3 months after a course of radiation is completed (usually after 6 months or sometimes years after treatment completion). Serious complications such as strictures are rare with FRT (risk ~2-4%)
- Urinary incontinence: around 30% of patients may exhibit some degree of permanent urinary incontinence after treatment, based on one study of around 50 dogs. In most of these cases, this was in the first 4 months after RT completion. The cause is unknown and in some dogs, it may have been due to a tumour rather than RT directly. In some dogs, this was mild and manageable and in some, it resulted in the necessity to use doggy diapers (nappies)
- Leukotrichia: white hair regrowth in the radiotherapy treatment site is normal but not common in dogs with bladder tumours
- Stricture (urethra): narrowing of the urethra leading to difficulty in urination or obstruction – may require medication or a procedure such as a stent
- Stricture (ureter): narrowing of the ureter leading to urine buildup in the kidney (hydronephrosis) causing kidney damage in some cases. May require a procedure such as a stent
- Stricture (colon/rectum): narrowing of the colon/rectum which may cause difficulty passing a stool/straining. May need dilating and anti-inflammatory medication or other therapy
- Radiation-induced tumours: an exceedingly rare complication (typically seen years after initial treatment) and is usually the development of a tumour arising within the treated site
The goal of radiotherapy is to reduce the risk of serious late side effects as much as possible – we aim for <5% overall however in certain individuals the risk may be higher (this will be discussed by your oncologist). The risk may be higher or not fully known, particularly in cases where a novel technique is being used or where SRT is being utilised.
What is the prognosis?
This is a very difficult question, as most bladder tumour studies have evaluated pets with various sizes/shapes and locations of their bladder/prostate tumour, some with metastasis and some without and using different radiotherapy protocols and doses. Also, in the studies looking at the outcome of RT, some pets have received radiotherapy alone, some as first-line treatment with/without chemotherapy and somewhere RT was used as a “rescue” treatment after chemotherapy has already been utilised. Because RT is a relatively new treatment for TCC, most older studies look at chemotherapy alone.
Broadly speaking, some median survival times (MSTs) are outlined below. Median survival is similar to the average. It means it is the time at which 50% of patients have died of their tumour, and 50% are still alive:
- NSAID alone: 3-6 months
- NSAID + chemotherapy: 6-12 months
- NSAID + definitive-intent radiotherapy (+/- chemotherapy): 14-22 months
These are not set in stone, but looking at the available studies, the more intensively we treat this type of cancer, the better the outcome.
Unfortunately, no guarantees come with any type of cancer therapy. Very rarely, some patients develop cancer spread very quickly after treatment.
Some types of prostate cancer (adenocarcinoma) in dogs can spread very quickly and aggressively and behaves differently than TCC described so far. Unfortunately, in localised cases of prostate cancer at diagnosis, it can be impossible to know whether a tumour will behave more like a TCC or more like a prostate adenocarcinoma. Therefore there is a bit more “risk” associated with the treatment of prostate tumours – as some will not do very well at all. In one study, tumour involvement of the prostate in male dogs was associated with shorter survivals.
The goal of palliative-intent radiotherapy is to improve symptoms rather than extend survival significantly – but this can still buy some pets a few months of being more comfortable.
Chemotherapy:
As discussed earlier, this was (and for some oncologists still is) traditionally the “standard of care” for dogs with urogenital TCC. The downside of chemotherapy is that as it gets everywhere in the body, it can potentially cause toxicity to various organs in the body – so the dose has to be kept relatively low. In contrast, as RT is a localised treatment and most TCCs are localised initially, a much higher dose can be given to the tumour which will therefore have a much better chance of tumour control.
The fact that chemotherapy, unlikely RT, gets everywhere in the body is also its upside. It may get rid of any tumour cells that might be lurking in other organs (lung, liver, bone) that may form metastases (secondary cancer tumours) later on. Therefore, we tend to recommend some chemotherapy after radiotherapy with the hope that it will a) help kill some of the cancer cells in the urinary tract in addition to RT and b) help to delay/prevent the cancer from spreading elsewhere in the body.
When chemotherapy is used as a sole treatment (without RT) we typically start with one drug and monitor its effectiveness (e.g. with ultrasound) after a few treatments. If it works, we tend to carry on indefinitely. If it doesn’t work or stops working, then we try a different drug. We keep going until no drugs work, there are no good drugs left or you decide you do not wish to pursue more treatment. Sometimes dogs can stay remarkably stable by receiving multiple, sequential chemotherapy drugs over a period of time; sometimes for many months. Unfortunately, in some dogs, chemotherapy doesn’t appear to make a massive difference to their symptoms.
If chemotherapy is given after radiotherapy, we tend to give a shorter course (e.g. 4-8 sessions, depending on the patient and drug) as the main role of chemotherapy is to delay/prevent tumour spread. The RT should have done a good enough job with the primary tumour in the urinary tract – so we don’t need to continue using it long-term unless the tumour progresses. Further chemotherapy may be recommended if/when the tumour comes back.
Palliative Care:
Should you not wish to proceed with any anti-cancer treatment, palliative care should be considered. Palliative care is where we treat the symptoms associated with the tumour without giving any direct anti-cancer treatment. We often recommend anti-inflammatories (NSAIDs) and/or painkillers, but the exact treatment will depend on the symptoms that your dog has.
What about cats?:
There is much less information about TCC in cats as it is rare. However, the general principles are similar and so the recommended treatment plan is likely to be similar.