Radiotherapy for
Brain Tumours In Dogs
Back to Fact Sheets
The two most common types of tumours we treat are meningiomas (most common) and gliomas.
Download PDF
What type of brain tumours do you treat? Is surgery useful?
The two most common types of tumours we treat are meningiomas (most common) and gliomas. We also treat pituitary tumours and less common types of tumours called choroid plexus tumours or nerve sheath tumours (NSTs). Pituitary tumours and NSTs are somewhat different to other types of brain tumours and are discussed elsewhere in another fact sheet.
Meningioma

Meningiomas are slow-growing, mostly benign tumours which arise from the meninges (envelope that surrounds the brain). Therefore they are located peripherally and usually have a typical MRI appearance. The most common symptom they cause are seizures, particularly when they are in the front of the brain. When they occur in the back of the brain, they often cause balance issues, a head tilt or turn, circling and/or leg weakness. If they occur in the very back of the brain/top of the spine, they can sometimes cause spinal pain. Meningiomas can be split into 3 grades: grade 1, grade 2 and grade 3. The lower the grade, the less quickly they grow, and the longer they take to grow back after surgery (if removed) and generally we expect the outcome with any type of treatment to be better, Luckily, high-grade (grade 3) meningiomas are much rarer, but they can grow quickly and occasionally will spread to other areas of the brain or extremely rarely to the lungs/other sites. We mostly don’t know what grade a patient’s tumour is because we rarely perform a biopsy and so usually only find out in patients that underwent surgical removal of their tumour.
It is important to note that even when meningiomas can be removed surgically, the outcome with surgery alone is not that great (~6-12 months) as usually not every single tumour cell can be removed, so these tumours often grow back. Radiotherapy (RT) is therefore usually recommended afterwards to try and sterilise the remaining tumour cells to try and prevent or at least delay tumour recurrence at the surgical site, Occasionally, if surgery is performed and the surgeon was very happy with the resection and the tumour was grade 1, cautious monitoring may be advised.
When it is feasible, brain surgery is not simple and can be a high-stakes procedure. Therefore, given pets can do well with RT alone, many owners decline surgery, even if it is possible.
Because many tumours are not easy to surgically remove and many owners do not wish to pursue surgery, radiotherapy alone is most commonly performed for canine meningiomas. To date, there is not really enough data to tell us whether surgery before RT improves outcomes compared to RT alone.
Surgery may be more strongly recommended before RT if the tumour is causing particularly problematic symptoms – e.g. a dog that has major mobility issues, particularly a large tumour causing intense seizures which are difficult to control medically or pain/weakness due to a spinal meningioma. In such cases, surgery will immediately remove the tumour and possibly reverse the associated symptoms. The pet may therefore be happier and also better able to tolerate anaesthesia for RT.
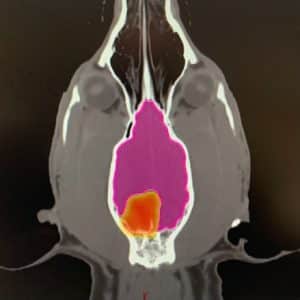
Glioma

Glioma is an umbrella term for a group of tumours that arise from the brain tissue itself – so they have a different appearance to meningiomas and are deeper in the brain. They vary from small, slow-growing tumours to aggressive masses which quickly compress the brain and cause surrounding swelling, resulting in potentially fatal consequences. Some MRI features can help us predict (only in some cases) whether a glioma may be a higher or lower grade (i.e. more or less aggressive, respectively) but this is not perfect and there is no way of knowing other than biopsy. A biopsy is rarely performed as it usually doesn’t change the recommended treatment and so for most owners doesn’t justify the risks and expense. This marked variation in behaviour makes it very difficult to predict the outcome of an individual patient with a glioma.
Due to their deep position and the difficulty in differentiating brain and tumour tissue at surgery, radiotherapy alone is the most common treatment recommendation. Surgery is rarely performed.
These tumours are uncommon and there is very little data regarding their outcome with RT, Surgery is almost never performed as they are right in the centre of the brain. These tumours usually reside within the ventricular system (the fluid-filled spaces within the brain). Frequently there is a build-up of too much fluid in the brain (“hydrocephalus’), secondary to the tumour obstructing the normal drainage pathways. This results in excessive pressure in the brain which can have serious neurologic consequences. Sometimes, this renders the anaesthesia required for RT too risky, and a “shunt” may be recommended prior to RT (a special tube which is surgically placed and drains the excess fluid to the belly). In patients that get through their RT protocol, the long-term outcome can be as good as other brain tumours.
Radiotherapy
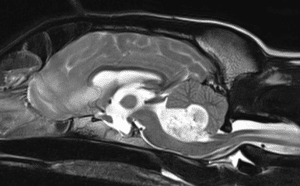
Radiation therapy involves treatment with high-energy X-rays, the aim being to kill the tumour. We use a machine called a linear accelerator, Patients lie on the treatment couch and the machine delivers a focussed beam of X-rays from multiple angles 360° around the patient.
Each radiation treatment is performed under a short, light general anaesthetic. Before the start of treatment, a planning CT scan (and sometimes an additional MRI if stereotactic radiation is recommended) will be needed to help us prepare a bespoke plan for your pet. This helps us to maximise the radiation dose to the tumour whilst sparing the nearby tissues. This will be required even if your pet has had a recent CT scan, as we need patients to be in a very particular and fixed position so that the treatment can be carried out with pinpoint accuracy.
Unfortunately, even with radiotherapy, we usually cannot cure your pet’s brain tumour. However, radiotherapy can be a very satisfactory treatment for improving quality of life, reducing the risk of side effects and controlling the tumour. RT is well tolerated by most patients; particularly with newer technologies to help avoid side effects and in many cases make treatment courses much shorter.
Do brain tumours spread to other places in the body?
Brain tumours rarely spread from their primary site. A very small number of aggressive tumours can spread to other areas of the brain and spinal cord. It would be extremely rare for a brain tumour to spread to other areas of the body but other age-related conditions can occur in the chest/abdomen (unrelated to the brain tumour) which may impact the management of your pet’s brain tumour (e.g. affect your/our decision or recommendation to pursue RT; should there be an important, unrelated finding). We typically recommend at least a chest CT at the time of your pet’s head CT scan (performed to plan RT), but preferably we would scan through the chest and abdomen (belly). The additional rationale for concurrent chest/abdominal imaging is the potential that the brain tumour is not a primary brain tumour, but there is a different tumour in the body that has spread to the brain (i.e. the brain tumour is actually a metastasis).
Will my pet still have seizures or other tumour-related symptoms after RT?
Brain tumours are sensitive to radiotherapy, though the response can be different for each patient.
The full effect of the treatment may be slow and can take months for the tumour to slowly shrink to the smallest size. Some tumour types shrink more slowly and shrink less. In some patients, we might only be able to stop it from growing further.
Overall, studies suggest that at some point after treatment, over 90% of affected pets will have an improvement in their symptoms and/or tumour volume reduction on a follow-up CT scan.
The hope is that as most tumours at least stop growing, any seizures or symptoms will not get any worse (whilst the tumour is under control). Many tumours do shrink with RT, so we hope that the risk of seizures reduces and any other symptoms relating to the tumour will improve. However, even where tumours shrink dramatically, any residual tumour or scar tissue in the brain could still act as a seizure focus (the focus of abnormal electrical activity in the brain). Therefore, most pets that presented initially with seizures continue to take anti-seizure medications long-term, unless there are any adverse effects. Steroids are usually weaned after RT, usually over several weeks or even months (varies depending on the case). Some pets will require a low dose of steroids long-term, or have a period off them and then need to go back on them.
Radiotherapy Protocols
There are several different types of radiotherapy protocols that we generally offer for dogs with brain tumours:
- Fractionated Radiation Therapy (FRT; this is the most conventional type of radiotherapy).The total radiation dose is split into multiple small treatments (called fractions) to ensure the radiation is not too damaging to any normal tissues around the tumour in the long term (mainly the brain). This treatment usually consists of 10-20 fractions, each given once a day (not weekends), over 2-4 weeks. The main acute side effects that can occur include some sore mouth, ear (on the side of the tumour) and sore eyes(s) (if near the tumour) for a couple of weeks after treatment finishes. We almost always use intensity-modulated radiation therapy (IMRT) if a brain tumour is close to a sensitive structure: a type of RT delivery which means we can significantly avoid radiation dose to the normal structures around the tumour. This means the degree and severity of acute side effects are massively reduced from what we used to see historically. Because the treatment is delivered as multiple smaller doses, the risk of late effects (see later), particularly to the brain, is very low. The goal of this protocol is to give the best tumour control possible
- Stereotactic Radiation Therapy (SRT). This is a newer type of radiotherapy technique which has come about due to significant technical developments in radiotherapy over the last few years. SRT usually consists of 3-5 treatments delivered once daily over 3-5 consecutive days (Monday to Friday; there are no treatments at weekends). It is a highly focused technique with the goal of treating the tumour but as little surrounding normal tissue as possible. The risk of acute side effects (see below) associated with this protocol is very low. There is an increased risk of an “early delayed” side effect of the brain (see below) compared with FRT. The risk of late side effects is at least the same as with fractionated radiation, if not a little higher due to the high dose given with each treatment. Therefore, this technique may not be possible for all tumours – particularly those that are very large, are not well-defined, have lots of surrounding inflammation or involve certain areas of the brain that are more sensitive
There is still some work to be done to try and ascertain whether FRT or SRT results in improved outcomes, and it likely depends on the tumour type. SRT appears equally effective to FRT when a mixture of tumours are compared, but some data suggest that SRT may not be quite as good for long-term survival in canine meningioma, SRT might be better for canine glioma and SRT does not appear particularly effective for many pituitary tumours (see later)
Either way, SRT is much more convenient for pets and humans due to significantly fewer treatments and anaesthetics. Therefore, some owners may choose this option despite in some cases it not being the “preferred” option – or we may recommend it because for some pets there could be a higher risk with multiple anaesthetics
- Palliative radiation therapy – this is when we give a low/modest dose of radiation to try and provide an improvement in symptoms but with short protocols and with little short-term (acute) toxicity. The goal/expectation is not long-term survival but to try and make pets more comfortable for the time they have left. Most protocols are once per day for 5 consecutive days, or once per week for 4-6 weeks. Sometimes the choice is based on tumour size/location/type and sometimes is based on owner preference
- Individual protocols: may be used in certain situations, for example, due to a patient’s concurrent medical conditions or temperament
Potential side effects related to radiotherapy:
Acute side effects (predictable and temporary)
- Hair loss (alopecia) in the treated site: very rare with brain tumours and not expected – potentially more likely in very tiny patients, particularly if they are a non-moulting breed
- Sore skin (radiation dermatitis): very rare with brain tumours and not expected
- Oral mucositis:rare with brain tumours and not expected but possible for tumours in certain locations (expected to be very mild)
- Eye side effects: conjunctivitis, ocular discharge, dry eyes, sore skin around the eyelids or inflamed/swollen eyelids (blepharitis). Very rare with brain tumours and not expected
- Vision changes: when brain tumours have caused vision loss, this may not be reversible and there is no way of predicting this. Radiation could cause some damage to the optic nerve (associated with vision) in the long-term but this is not common (may be more likely with SRT, when the optic nerves are nearby to the tumour)
- Death: This is extremely rare but pets with brain tumours can suddenly deteriorate during treatment due to tumour effects, anaesthesia (e.g. aspiration pneumonia) or brain swelling – we estimate that around 5% of pets may not make it through the treatment course
In brain tumour patients, these side effects are usually mild and rarely problematic these days. They are short-term, predictable and self-resolving.
“Early-delayed” side effects (much more common with SRT)
This is a syndrome where there is neurological deterioration (usually recurrence or worsening of the original presenting sign – e.g. seizures) around 1-3 months after receiving a course of RT. This is due to some changes in the nerve fibres of the brain and is usually reversible with steroids (anti-inflammatories) or an increase in the dose if pets are already on this. Unfortunately, in a small proportion, this side effect does not resolve/improve and results in a decision for euthanasia. The risk is very low with FRT (~5%) but can be as high as 20-30% with SRT (probably one of the biggest downsides of this treatment option).
Delayed complications – these are uncommon and typically arise 6 months or later (sometimes years) after treatment completion.
- Leukotrichia: white hair regrowth in the radiotherapy treatment site is normal (unusual with brain tumours)
- Cataracts: very rare with brain tumours and not expected to be vision-changing if they occur
- Neurologic changes: seizures, brain damage etc
- Radiation-induced tumours: an exceedingly rare complication (typically seen years after initial treatment) and is usually the development of a bone tumour arising within the treated site
The goal of radiotherapy is to reduce the risk of serious late side effects as much as possible – we aim for <5% overall however in certain individuals the risk may be higher (this will be discussed by your oncologist).
What is the prognosis?
This is a very difficult question, as most brain tumour studies have evaluated pets with various types of brain tumours (i.e. a mixture of meningiomas, gliomas, pituitary tumours and other rare types) together as one group. It also possibly depends on what type of RT a patient has received (i.e. standard radiation [FRT] versus SRT).
Prognosis is notoriously difficult for dogs with brain tumours. This is because the diagnosis of tumour type is not definitively confirmed (MRI is very good at predicting tumour type broadly, but is not perfect), there are various grades of meningioma and glioma which have different biologic behaviours (and we do not know these without biopsy) and these tumours arise in various anatomic locations within the brain, which cause various clinical signs from none to severe seizures, which are very difficult to control. Therefore, the outcome post-RT is very wide, from death due to neurologic progression during or shortly after the treatment course, to many years of survival.
Overall, most contemporary brain tumour RT studies show survival of ~1-3 years. Without treatment, the average survival time of dogs with brain tumours of any type tends to be around 2-3 months, but this is highly variable and depends on the location of the tumour within the brain and also the severity of neurologic signs.
More specifically:
Meningiomas
- FRT is generally recommended as the best option with typical published “median” survival times from recent/larger studies in the 18-24 months range
- SRT is also a good option for canine meningioma but overall the outcomes aren’t perhaps quite as good, with typical published “median” survival times in the 12-19 months range – though the optimal dose/regime is still being studied as this is a newer treatment
- Overall, both are very reasonable options to treat meningiomas, and there is a lot of overlap between the published outcomes with FRT and SRT
Gliomas
- Gliomas have different “grades” (how aggressive the tumour is when assessed under the microscope) which we usually do not know as a biopsy is rarely performed. High-grade gliomas have a worse outcome compared with lower-grade gliomas
- FRT tends to result in outcomes of 8-12 months when gliomas are assessed specifically, but in one study this was 26 months
- Two recent reports of SRT for glioma reported outcomes of 13-21 months, which suggests the outcome may be superior with SRT (but smaller tumours tend to be treated with SRT, which may do better and so bias the results in favour of SRT)
- Some gliomas will spread to other areas of the brain later on. This is rare (<10%) but can occur and it cannot be predicted
Choroid plexus tumours
- Rare so there is little data regarding the outcome of cases treated with RT published
- A shunt may be recommended before RT if there is a concern for very high pressure in the brain
- Some recent published data and our experience is that for patients that make it through a course of radiation, the outcome can be similar to other brain tumour patients
- A small proportion of these tumours exfoliate some of the tumour cells into the fluid that they sit in, which spread to other areas of the brain or spinal cord and can cause problems later (so-called “drop metastases”)
Chemotherapy:
This is usually the least satisfactory treatment for pets with brain tumours. Multiple conventional injectable drugs have been previously used; however, the success is relatively limited compared with RT and most chemotherapy drugs don’t penetrate the brain very well.
Meningiomas have rarely been reported to respond to certain chemotherapy agents, but they are rarely used.
One study suggested that dogs with glioma treated with chemotherapy (lomustine) lived longer than those that didn’t receive chemotherapy (138 days versus 35 days). This is potentially an option for some pets and their owners. Some other drugs (e.g. temozolomide) have also been utilised alongside radiotherapy, but the contribution of chemotherapy to the outcome is unknown.
We are happy to discuss this option with you if you wish to consider chemotherapy for your pet.
Palliative Care:
Should you not wish to proceed with any anti-cancer treatment, palliative care should be considered. Palliative care is where we treat the symptoms associated with the tumour without giving any direct anti-cancer treatment. We often recommend anti-inflammatories (steroids) and/or painkillers, but the exact treatment will depend on the symptoms that your dog has. Seizure medications are common and many dogs with brain tumours have seizures as a major presenting symptom. The survival time for patients treated with palliative care can range from a couple of weeks up to a few months, depending on the impact of the tumour on their quality of life. Typically the outcomes are around 2-3 months.


