Spinal Arachnoid
Diverticulum (SAD)
Back to Fact Sheets
Information for pet owners on the causes, symptoms, diagnosis and treatment for spinal arachnoid diverticulum (SAD) in dogs.
Download PDF
What is an SAD and why does it occur?
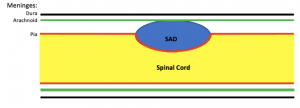
A spinal arachnoid diverticulum is pouch of fluid within the subarachnoid space, which is located between the meninges. The meninges are thin layers of tissue surrounding the brain and spinal cord. The location of an SAD is shown on the diagram below, depicting the spinal cord of an affected dog, viewed from the side:
Rottweilers, Pugs and French Bulldogs are most commonly affected. The cause of SAD development is not fully understood. Possibilities include a congenital abnormality (i.e. a problem the animal was born with), or that they occur secondary to some other spinal disease such as trauma, inflammation, intervertebral disc disease, or malformation of the bone or joints of the vertebral column. This is particularly true of French Bulldogs and Pugs, whereas Rottweilers very rarely have evidence of a concurrent spinal disorder. It may be that a combination of genetic susceptibility and environmental factors leads to SAD formation.
What signs do dogs with a SAD show?
The clinical signs (symptoms) can appear at any age. In large breeds, they tend to occur in young adulthood, whereas in other breeds, such as pugs, they are more typically seen in middle age.
The signs shown by the dog are caused by compression on the spinal cord by the SAD. Essentially, the compression prevents messages travelling up and down the spinal cord correctly. The exact signs depend on the location of the compression. If the SAD is located in the neck, which is more common in large breeds such as the Rottweiler, the dog may be ataxic (uncoordinated) and be unable to generate normal movements on all four legs. If the SAD is in the middle of the back, which is more common in smaller breeds such as pugs, the back legs may appear ataxic and not move normally. Urinary and/or faecal incontinence may occur. This is because the messages telling the dog it needs to pass urine or faeces do not make their way up the spinal cord to the brain normally, meaning the dog is unaware that it needs to go.
The signs tend to gradually get worse with time. The condition is not usually painful.
How is an SAD diagnosed?
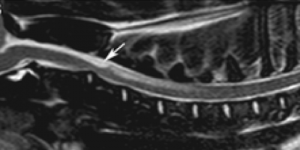
An MRI scan is the method of choice to diagnose an SAD. This allows the SAD to be visualised and also rules out other possible spinal cord diseases that may present in a similar way to an SAD. The typical MRI appearance is a rounded, fluid-filled abnormality, usually located on top of the spinal cord, with a characteristic teardrop shape, as indicated by the arrow in the image below:
Once the diagnosis of an SAD has been reached, further diagnostic tests may be recommended in order to look for abnormalities that might have predisposed the SAD formation. Such tests might include a CSF tap, which involves taking a sample of the cerebrospinal fluid that surrounds the brain and spinal cord to look for evidence of inflammation, and a CT scan to evaluate abnormalities of the bones or joints.
What treatment is required?
Surgery is the recommended treatment for SAD. A window will be made in the bone overlying the SAD. The SAD can then be drained and a portion of its wall removed, so that the spinal cord is decompressed. If there is evidence of an underlying cause for the SAD formation, it may be possible to address this at the same time. For example, some dogs have underdeveloped joints between the vertebrae, making them unstable. This instability is thought to be a trigger for the SAD formation. In these cases, implants may be placed to stabilise the vertebrae, to reduce the risk of SAD recurrence.
If surgery is not possible, anti-inflammatories and physiotherapy can be attempted to try to slow the progression of the disease.
What is the prognosis?
Up to 80% of dogs improve following surgery, though transient post-operative deterioration is very common. Recurrence of clinical signs has been reported in around 20% of dogs. One possible cause of recurrence is not addressing predisposing factors such as vertebral instability, which is why it is so important to thoroughly investigate this prior to planning surgery.
With medical treatment, improvement is only seen in around 30% of cases and unfortunately, deterioration is more typical.


